Hidden Dangers: How Heavy Metals Contribute to Osteoporosis and what to do about it
/When we think of osteoporosis, we often point to aging, hormonal changes, or calcium deficiency. But what if an invisible threat has been quietly undermining your bone health? Enter heavy metals—toxic elements like lead, cadmium, aluminum, and mercury that can silently accumulate in the body and wreak havoc on your skeletal system.
The Silent Intruders: What Are Heavy Metals?
Heavy metals are naturally occurring elements found in the earth’s crust, but modern industry has drastically increased our exposure. From air pollution and cigarette smoke to contaminated water and food, these metals find their way into our bodies. Unlike essential minerals, heavy metals serve no positive biological purpose and can disrupt vital physiological functions.
How Heavy Metals Harm Your Bones
Lead (Pb): The Calcium Impersonator
Lead mimics calcium and gets stored in your bones. Over time, it interferes with bone remodeling, weakens bone structure, and even leaches out during times of stress or hormonal change, compounding bone loss.Cadmium (Cd): The Kidney Saboteur
Cadmium exposure, especially through smoking or industrial pollution, not only damages the kidneys but also reduces calcium reabsorption and disrupts vitamin D metabolism—a perfect storm for osteoporosis.Aluminum (Al): The Bone Builder’s Blocker
Found in certain medications, cookware, and processed foods, aluminum hinders the activity of osteoblasts (bone-forming cells), essentially halting new bone formation.Mercury (Hg): The Disruptor
Mercury accumulates in soft tissues and can cause oxidative stress, inflammation, and mineral imbalances that indirectly erode bone density over time.
Mechanisms of Damage
Oxidative stress: Heavy metals increase free radicals, damaging bone cells.
Hormonal disruption: They can interfere with vitamin D, parathyroid hormone, and estrogen.
Mineral displacement: These metals replace bone-strengthening minerals like calcium and magnesium.
Reducing Exposure and Reclaiming Bone Health
Test, Don’t Guess
Consider lab testing (hair, blood, or urine) to assess heavy metal levels.Support Detoxification
Nutrients like glutathione, selenium, zinc, N-acetylcysteine (NAC), and alpha-lipoic acid help your body eliminate toxins more efficiently.Filter and Choose Wisely
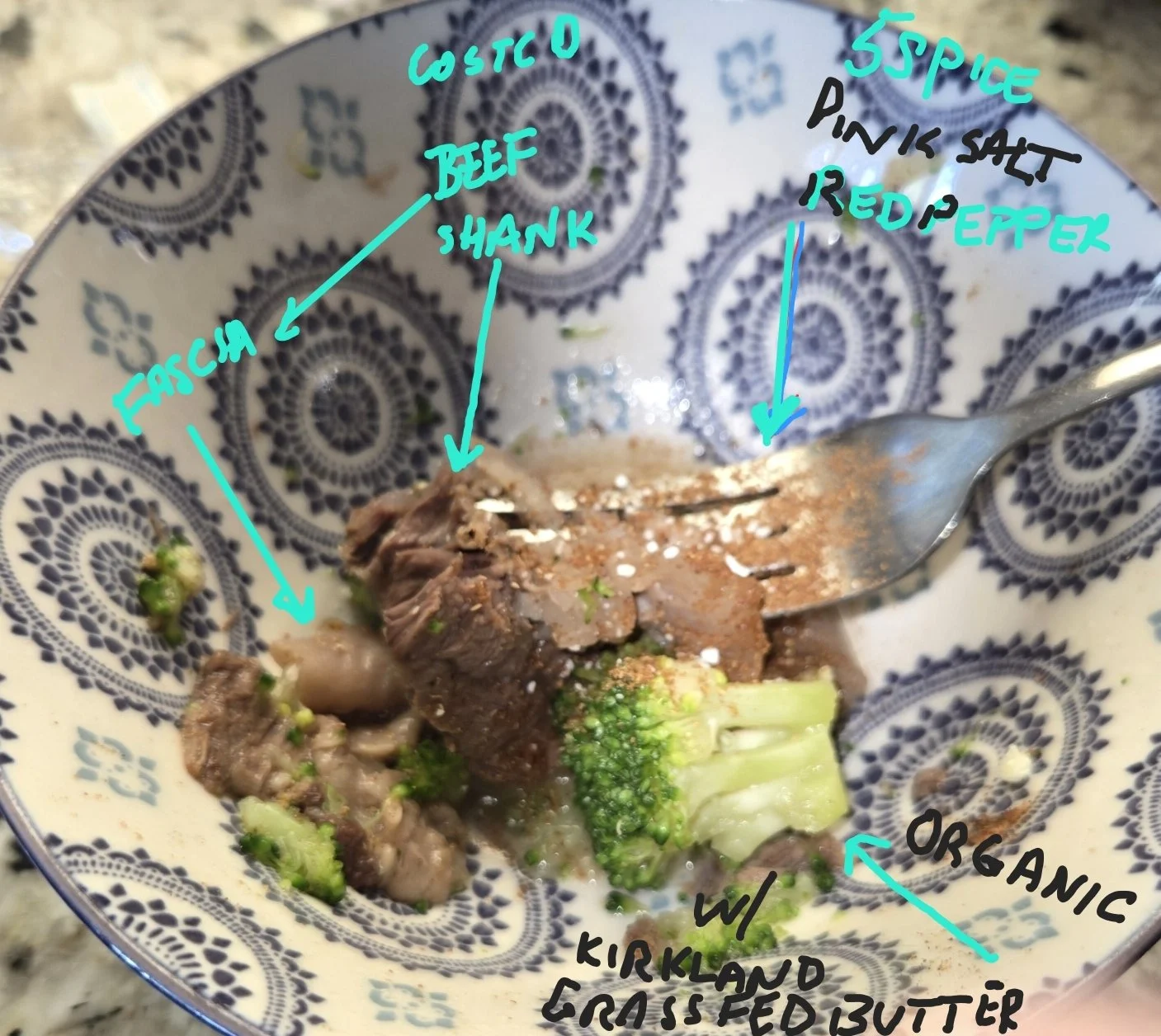
Use water filters, avoid aluminum cookware, and opt for low-mercury fish like salmon, sardines, and anchovies (S.M.A.S.H. fish).Strengthen Your Bones
Prioritize weight-bearing exercises, vitamin D3, magnesium, K2, and clean calcium sources.
Final Thoughts
Bone health is about more than just calcium supplements. In a world full of hidden toxins, being aware of heavy metals and their silent role in osteoporosis could be the game-changer your wellness routine needs.
Knowledge is power—and in this case, it might just be the power to prevent a fracture and reclaim your health.
Assessing organic acids can provide valuable insights into metabolic processes that may influence bone health, including osteoporosis related to menopause. Organic acids testing (OAT) evaluates various biochemical markers in the body, which can highlight potential imbalances that affect bone health, such as:
1. Nutrient Deficiencies
Organic acids can indicate deficiencies in vitamins and minerals essential for bone health, such as:
Vitamin D (crucial for calcium absorption).
Vitamin K2 (important for directing calcium to bones).
Magnesium (essential for bone mineralization).
B-vitamins (involved in reducing homocysteine, which can affect bone density).
2. Oxidative Stress
High oxidative stress markers in an OAT can suggest increased free radical activity, which may impair bone remodeling and increase the risk of osteoporosis. Antioxidants like glutathione and coenzyme Q10 can help mitigate this.
3. Inflammation
Certain organic acids are linked to inflammation, a process that can accelerate bone resorption (breakdown). Reducing systemic inflammation can improve bone health.
4. Gut Health
Imbalances in gut bacteria can affect nutrient absorption, including calcium, magnesium, and vitamin D. Organic acids testing can detect dysbiosis and guide gut health interventions.
5. Hormone Metabolism
Menopause reduces estrogen, a hormone that protects bone density. Organic acids related to neurotransmitter and hormone metabolism (like serotonin and dopamine pathways) can reflect stress or adrenal dysfunction, indirectly impacting bone health.
6. Detoxification Pathways
Organic acids can reveal issues with detoxification, particularly of estrogen metabolites. Supporting liver health may improve estrogen metabolism and protect bones.
Actionable Steps Based on OAT Results
If imbalances are detected, interventions may include:
Dietary changes: Increasing calcium, magnesium, and vitamin D-rich foods.
Supplements: Addressing deficiencies with specific nutrients like Vitamin D3, K2, and magnesium.
Lifestyle: Weight-bearing exercise and stress management to support bone remodeling.
Gut support: Probiotics, prebiotics, or addressing dysbiosis if indicated.
Hormonal support: Bioidentical hormone replacement therapy (BHRT) or phytoestrogens.
Organic acids testing can thus serve as a functional tool to personalize osteoporosis prevention and treatment plans during menopause.